Home Health Services Coverage
Table of Content
- Medicare Home Health Care Coverage
- Is private duty covered by insurance?
- Is home health care covered by Medicare A or B?
- How Do I Learn More About UnitedHealthcare and Home Health Care Coverage?
- Examples of skilled home health services include:
- How Much Do Home Care Services Cost
- Home health covered services
Most forms of private insurance will not pay for non-medical home care services, and in-home skilled care is rarely covered at 100 percent. Skilled nursing care includes treatments that require specific knowledge and training to administer or complete. Treatments must be needed part time, at least once every 60 days, but not more than once daily for up to three weeks. Medicare will cover home health care for homebound seniors if they have been prescribed that care by a medical professional.
Medicare will also count a person as homebound if a doctor advises them to stay at home because of a medical condition. For instance, Medicare covers the expense of renting some items of equipment. Medicare will also reimburse the cost if patients decide to purchase the device.
Medicare Home Health Care Coverage
The information on this website may assist you in making personal decisions about insurance, but it is not intended to provide advice regarding the purchase or use of any insurance or insurance products. Healthline Media does not transact the business of insurance in any manner and is not licensed as an insurance company or producer in any U.S. jurisdiction. Healthline Media does not recommend or endorse any third parties that may transact the business of insurance.
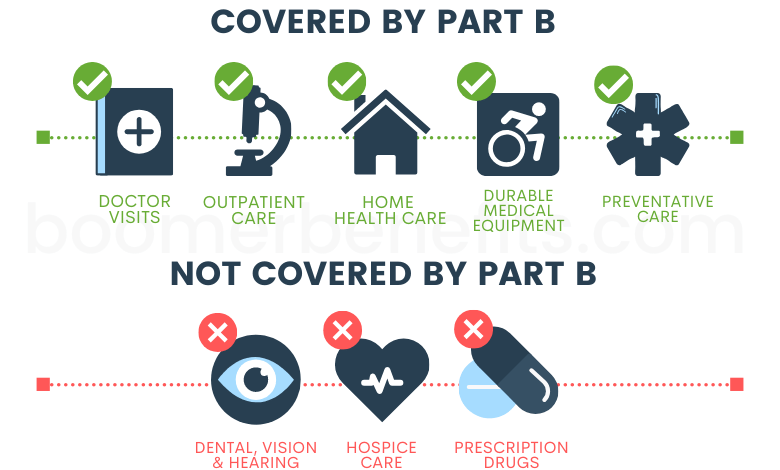
Note that you cannot participate in the PAS program if you qualify for any of Virginia’s Medicaid waiver programs. For example, letâs say your doctor arranges for home nursing and physical therapy visits to help you recover from a stroke. Original Medicare covers eligible home health care services at no cost to you if you meet certain requirements. For eligible durable medical equipment , youll pay 20% of the costs after meeting your Part B deductible. If you need more than part-time or intermittent care, you will not be eligible for home health care benefits. Custodial care includes non-medical services and activities of daily living, such as bathing, dressing, and household chores like cooking and laundry.
Is private duty covered by insurance?
Skilled nursing services are those that must be provided by a qualified health professional, such as a Registered Nurse or a Licensed Practical Nurse . Ask your home health agency how much Medicare will pay before you begin receiving home health care. This can help prevent you from being surprised by unexpected out-of-pocket costs. WellCare and UnitedHealthcare are both popular insurance companies that sell Medicare plans in many ... Medicare Supplement Insurance, or Medigap, supplements your Original Medicare benefits by covering your Medicare out-of-pocket expenses like copayments, coinsurance and deductibles. Skilled care refers to care that can only be administered by trained health care professionals, such as physical therapy.
The treating physician must certify that the beneficiary requires intermittent nursing care, occupational treatment, speech therapy, physical therapy, or all four. The home health aides must work for a Medicare-approved home health agency and your doctor must certify that you arehomebound. These agencies agree to be paid the Medicare-approved amount and to be paid directly by Medicare. The home health agency will be responsible for all of your medical, nursing, and rehabilitative care and will communicate your needs to the managing physician.
Is home health care covered by Medicare A or B?
Home health services include home health nursing, home health aide, and skilled therapies . The only provider of home health services is a Medicare Certified Home Health Agency . Information provided on Forbes Health is for educational purposes only. Your health and wellness is unique to you, and the products and services we review may not be right for your circumstances. We do not offer individual medical advice, diagnosis or treatment plans. Your kidney doctor bills separately for the Medicare-covered ESRD services you get as an inpatient.
You also don’t need to get the drugs that are included in the bundle from your Medicare drug plan . The Advance Beneficiary Notice is a verbal and written breakdown of fees provided by the home health agency. In order to validate that the services are covered by Medicare, a home health agency may do so in some states.
Before home care services can begin, VNS Health will provide a written estimate of how much of your bill should be covered by Medicare, as well as which items and services are not included in the coverage and their costs. Besides Medicare and Medicaid, there are several programs and government aid options to help cover the costs of home care. Each has its own eligibility requirements and list of services it will cover. In addition, paying out of pocket is always an option, though many people will quickly find this cost-prohibitive without a plan to raise enough cash.
If your doctor recommends home health and you live in one of the states mentioned above in the U.S, you should immediately request the pre-claim review to know if you have to pay for the services. Christian Worstell is a senior Medicare and health insurance writer with MedicareAdvantage.com. Christian is well-known in the insurance industry for the thousands of educational articles hes written, helping Americans better understand their health insurance and Medicare coverage. Every Medicaid program in every state has its own eligibility considerations. Generally speaking, most adult day care is provided under Medicaid waivers.
A doctor can deem that youre homebound if he or she believes that your illness or condition could get worse if you left the home. Medicare will pay for whats considered intermittent nursing services, meaning that care is provided either fewer than seven days a week, or daily for less than eight hours a day, for up to 21 days. Sometimes, Medicare will extend this window if a doctor can provide a precise estimate on when that care will end. Not all Medicare Advantage plans offer these benefits, and those that do may have limitations on how the benefits can be used. For example, the plan may choose to cover up to 50 hours per year of home health aide services, or 20 transportation trips per year.
Intermittent nursing involves under 8 hours of care a day for 21 days or, in some circumstances, up to 35 days. It can also refer to nursing care that a person receives on fewer than 7 days of the week. Your home health agency, which will work with you during this time, can also tell you which services Medicare covers and to what extent. If the agency gives you any “extra” supplies or services not covered by your insurance, it’ll let you know by giving you a notice called an Advance Beneficiary Notice . Some Medicare Advantage plans provide further coverage for home health services, and this information should be included in your explanation of benefits.
Comments
Post a Comment